Fees and FAQ
You have questions, we have the answers!
Session Fees
Fees will be established at the first session and payment is to be made at the conclusion of each session. A receipt will be provided for you to submit to your insurance company or to use on your personal income tax. Methods of payment that are accepted are: cash, credit card (MasterCard or Visa), cheque, or e-transfer. Each therapist at Turning Point Counselling Collingwood determines his/her own fee.
You may have an extended health plan through your place of employment. Check with your therapist prior to the first session as to whether they direct bill to that plan. If they do not then you will be required to pay for the session yourself and then seek reimbursement from your insurance plan. Additionally, please check with your plan that they do cover therapy services provided by registered social workers. All of our therapists have Masters of Social Work degrees.
*Social Workers in Ontario are not required to collect HST on their therapy work, so there are no additional taxes added to our fee.
FAQ
General
Do you offer me a choice of in-person or online sessions?
Yes. Most of our therapists work both online and in-person. When we first talk with you we can help you understand the benefits of both kinds of session delivery, and align you with a therapist that works in your preferred way.
How can I access my therapy session?
We strive to be accessible, so sessions can be offered by telephone, secure video, or in-person.
Are the therapists at Turning Point qualified to provide counselling and therapy?
Our therapists are all registered social workers through the College of Social Workers and Social Service Workers. We all have graduate degrees in social work and years of specialized training, clinical supervision and experience. Cumulatively, among all our therapists, we have over 100 years of clinical experience!
How much do sessions cost?
Fees are determined by the therapist, and range from $120 to $150 per 50-60 minute session
Do I need a referral from my Family Physician or Nurse Practitioner?
Clients can self-refer to our Practice; however we do receive a significant number of referrals from primary health care practitioners, and other health and wellness service providers.
Can I see a male or a female therapist, if I have a preference for one over the other?
In our first conversation with you we will ask you if you would prefer a male or female therapist. It is important that you align with your therapist as a safe person, who is easy to talk to. We do everything we can to facilitate that.
Referral Process
Requests for counselling and therapy sessions can be self-referred through our Reach Us page. A referral from a medical doctor or psychologist is not required. We will respond to your request within one business day, and will work hard to connect you with a therapist that aligns with your counselling needs.
Privacy and Confidentiality
We take your privacy seriously. We adhere to the professional and ethical standards set out by the Ontario College of Social Workers and Social Service Workers (OCSWSSW). Personal, and personal health, information that has been provided to Turning Point Counselling will be secured with the utmost of confidence and all records will be stored in compliance with the Personal Health Information Protection Act, Ontario (PHIPA).
Payment Methods
We accept most major credit cards, e-transfer, and cash. Many of our clients are able to have their counselling covered by their health insurance plan. A receipt, which includes your therapist’s registration number and designation, will be issued within 24 hours of receiving your payment.
COVID
Will my therapist be fully vaccinated for the COVID-19 virus?
Yes, all of our therapists are fully vaccinated.
What are your procedures for ensuring the safety of clients from the transmission of COVID-19?
Clients and therapists are required to wear a mask at all times in the building. Our complimentary footwear is sanitized after use. Sanitization of surfaces is practiced daily.
COVID and Vaccinations
All of our therapists are fully vaccinated. Our rooms are consistently and frequently sanitized, and we have face masks and hand sanitizer located conveniently on site for clients as they enter the building. To ensure the safety of clients and therapists we ask that clients self assess for COVID-19 related symptoms, as well as cold and flu symptoms, prior to their scheduled appointment. For ease of accessibility we offer both in-person and virtual sessions.
Child & Youth Counselling
Do you provide child and youth biopsychosocial or psychoeducational assessments?
No. To obtain formal assessments, you will need to consult with a psychologist. The ways to find a psychologist include:
- Talk with the child’s school regarding the possibility of seeing a psychologist that works with the school board. This is paid for by the school board, however there are often long waitlists.
- Seeing a psychologist working in private practice, which is usually the quickest option. In many cases, a family member’s extended health plan may cover some of this expense.
What are signs my child is experiencing poor mental health?
If your child is having difficulty sleeping, performing everyday tasks, like going to school and doing things they would normally enjoy, it may be time to initiate a conversation with your child. Sometimes children with poor mental health are also more likely to engage in conflicts, have random aches and pains, and withdraw from friends and family.
What are ways I can help my child to have a healthy self-esteem?
Praise your child for their efforts, not just when they have successes. Encourage positive relationships, help them identify their strengths, show them they are valued and loved, encourage them to take risks and try new things, help them show kindness and compassion to themselves, and assist them in developing problem-solving skills and resilience.
My teenager just told me they have been self-harming and have been having suicidal thoughts. What are my options?
If you have a Family Physician or Nurse Practitioner, it’s a good idea to make an appointment with them first. CMHA has a 24 hr crisis line, as well as mobile support for youth over the age of 16 years old: Local 705-728-5044 or Toll Free 1-888-893-8333. KidsHelp Phone is also available 24/7, and has both phone and texting capabilities. Text CONNECT to 686868; Phone: 1-800-668-6868 or live chat at Get Support – Kids Help Phone
As we are not a crisis response, once your child is stabilized, you can contact us and we will set up a consultation with you.
How old does my child have to be to access counselling?
We offer counselling to children 6 years and older. Parents/Guardians of children and youth may be asked to join in sessions periodically, and for the initial session. Active ongoing communication with parents/guardians may be an expectation, especially for younger children. You may be asked to present court documents, and proof of child custody arrangements. Where there is joint or shared custody, both parents will be required to consent for children under the age of 12 years.
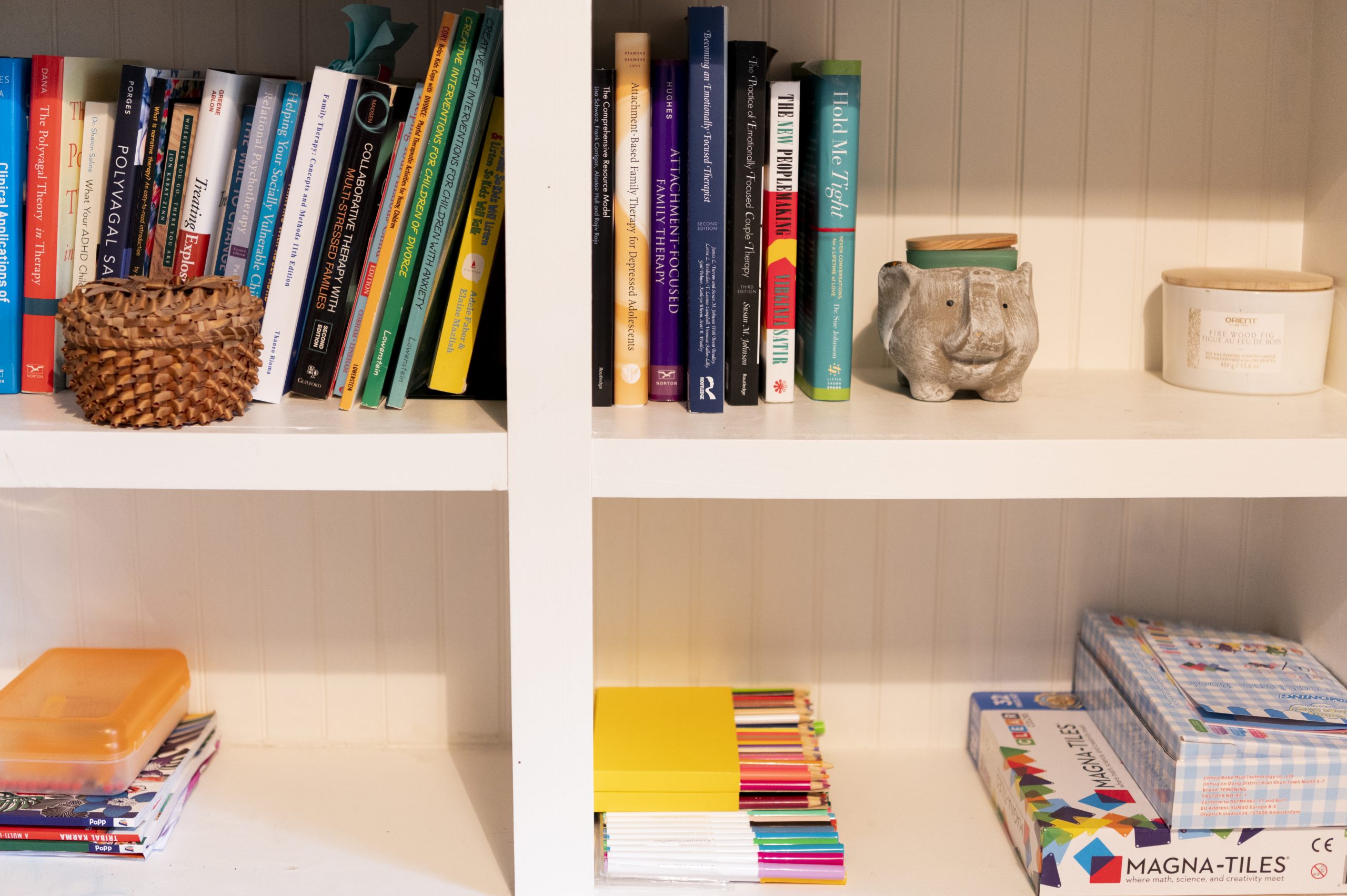
How different is child and youth therapy from adult therapy?
It differs in the use of language and complexity, and is geared to the developmental needs and abilities of the child or youth. Creative play and artistic activities are often used to guide the session.
I’ve booked my child’s first counselling appointment. How do I explain to them what is going to happen?
“We’re going to see (name of therapist). Her/His job is to help kids ___________ (describe briefly the situation). I’ve talked to the therapist and I think you’ll like her/him. You can talk to her/him about anything, and you will be doing some interesting activities!”
I would like my child to access counselling, but they don’t want to. Can I make my child go to counselling?
It’s always preferable if your child agrees to go to counselling and is willing to participate. However, if your child is refusing to attend their appointment, ask your child about their worries. Explaining to your child that this is a safe, private space for them to talk about what they want to someone who cares about them, may be helpful.
Couples Therapy
How can the therapist ensure I’m not going to be blamed, or the therapist won’t take sides?
A marital or couple’s relationship can often be experienced where one person feels blamed. Couples, however, get into a pattern of protection and activation and this prompts both individuals to become defensive. Good couples therapy doesn’t look for someone to blame. Rather, a couples therapist will help people identify the negative cycle, and help them to develop the skill to stay connected, avoid reactive behaviour and restore trust and communication.
Do you help high-conflict couples?
The first step in couples therapy is to help couples recognize their emotional raw spots, and begin to build safety. Conflict in an intimate relationship feels so destructive. Finding other ways to listen and be heard, to restore emotional safety and to begin to communicate your needs again are the first steps in the couple’s therapy process.
Will we be able to have couple therapy virtually if we are in two separate locations?
Yes. Couples therapy can be quite effective if done online. It works well even if the couple are in two different locations.
Is couple therapy appropriate if we just want a tune-up?
Couples therapy is effective for all couples; you don’t need to be in distress for it to be useful. Staying connected emotionally to your partner is essential for intimacy to be maintained. Sometimes just having a safe space in therapy permits couples to have honest and authentic conversations with each other again.
Can therapy be useful for couples who are separating and divorcing?
Working with a therapist can help people to safely manage the very intense emotions that accompany this process. Noticing the patterns of interaction, defining raw spots and painful vulnerability, can equip couples with the means to stay focused on the change in their family. For couples with children, with an ongoing commitment to co-parenting, therapy can open up opportunities to explore positive communication and help them to avoid the harmful cycles of emotional activation with each other.
Anxiety and Depression
How does generalized anxiety disorder differ from general anxiety?
Generalized anxiety disorder (GAD), is distinguished from general anxiety by persistent, excessive, and unrealistic worry about everyday things. Individuals with GAD, tend to have exaggerated worry, and think about worst case scenarios even if there is no evidence of this. Anxiety may feel very intense, and persistent. It might feel like you have no control over your worry, and its’ interruption of your overall health and well-being. You do not need to have GAD in order to access counselling for anxiety-related concerns.
I have both anxiety and depression. Which one should I treat first?
Many individuals experience both anxiety and depression. There are likely numerous factors that are contributing to both issues. However, generally speaking, chronic anxiety and worry can lead to avoidance of life circumstances and particular situations, including one’s own thoughts and feelings, which often leads to depression over time.
What is depression?
Depression is a mood condition that negatively impacts one’s thoughts, feelings, and behaviours. Depression can be persistent, short or long-lasting, and can significantly interfere with daily functioning. Untreated, major depression can sometimes lead to suicidal thoughts, and/or self-harming behaviours.
Trauma
What are symptoms of post-traumatic stress?
Symptoms can consist of flashbacks, nightmares, panic attacks, a high level of alertness, irritability or anger, little interest or pleasure in doing things, lack of concentration, restlessness, and an avoidance of activities and particular situations that remind the individual of the traumatic incident.
Do I have to revisit all of the details of my trauma?
No, trauma research has shown us that we do not need to talk about the details of our trauma experience for effective change to happen. We are more interested in hearing about how you presently think about your trauma, and other important aspects of your life.
When does a trauma experience(s) become post-traumatic stress disorder?
Not everyone who has experienced trauma has PTSD. When an individual experiences a traumatic event, there is an activation of emotional, physical, and brain-based responses. There are a myriad of biological, genetic, psychological and environmental factors that can contribute to the non-recovery or recovery of trauma.
My trauma happened years ago. Why is it still impacting me?
Trauma triggers the brain’s fight-flight-freeze response system. This is when the mind detects the threat and sends an automatic message to the body to move or freeze, which creates a rush of stress hormones that produce physiological changes to fight off the perceived threat to one’s safety. After trauma, the body holds the memories of the traumatic experience, and these can cause a number of physiological, and psychological symptoms well after the traumatic event.
Grief and Loss Counselling
When is grief and loss therapy or counselling needed?
Grief and loss counselling can be offered soon after the death to facilitate support to the individual or family who is grieving. Grief therapy, however, is not recommended until at least three months after loss, as typically bereaved individuals are still in shock and disbelief and may find it difficult to process their experiences with grief.
What is the main goal of grief and loss counselling and therapy?
To help the individual integrate the reality of the loss into their life, so that they can develop a new ongoing relationship with their loved one. Additionally, the bereaved individual is encouraged to learn and practice how to provide care to themselves so when grief surfaces they can tend to their sorrow in healthy ways.
Family Therapy
What would a family therapy session look like
Generally, the family therapy session would begin with the person, or persons, who made the referral for therapy. The therapist would seek to understand the nature of the problem, who was in the family structure and who would be interested in participating in the family therapy process. No one would be forced to be involved, but everyone interested would be able to have a voice in the definition of the problem, and become part of the process of change.
Would everyone in the family come to the first session?
Sometimes, but not always. It is helpful for the therapist to understand each perspective of the family problem, from each person or group. Parents might be in one session, children, if they chose to participate, in another. Then groups could be formed from there. Eventually it would be useful to have as many people as possible in the room, or at least be heard, including extended family and important others. This is a collaborative process between the family members and the therapist.
What if one or more people in the family choose not to attend?
Sessions can be very productive with everyone who chooses to attend present. Exploring the reasons why someone does not want to attend, and building more emotional safety for them, will often result in everyone being present and heard.
When should I think of family therapy?
Common requests for family therapy: when adult children are in conflict with their parents, or a sibling; when a family is trying to reconnect with cut off members of the family; when there is a family culture that is defined by conflict and intense emotion, such as a family with teen children; with families with younger children, who are too young for talk therapy themselves, then family therapy can begin to observe parenting styles, strength of the parenting team, stress from external forces such as grandparents, and mental health/substance use, for example.